Birth Story Part III: The Sacred Scar, 41 Hours of Labor and a C-Section
I never thought it would happen to me. The cascade of intervention I never wanted. Alchemizing Trauma. Spirituality guiding me before I even knew it.
Part 3—Induction and the Cascade of Intervention
Saturday night 2/24, my therapist took an emergency session with me. I shared with her all my fears and she ultimately reminded me of words mentioned from previous sessions about why I decided against a home birth. She said to me, “Your intuition knows you need to be at the hospital for whatever reason, trust that this is the right route for you.” In therapy, I came to the understanding that as much as I wanted a home birth, Saint Joseph’s Hospital in Denver, CO really did feel like the right place to birth my child. The hospital is highly awarded—rightfully so—and the values of birth aligned with mine: prioritizing skin-to-skin in post birth Golden Hour, jetted tubs to labor in, various birthing positions, no mom-baby separation unless medically necessary, dim lighting, aromatherapy, and high patient satisfactory. It felt like I could have the best of both worlds even though there’s no place like home. I felt safe and trusted my intuitive choice.
Read Part I Here and Part II Here.
A Timeline for 41 hours of Induced Labor, with and without the Epidural, Ending in a Cesarean Section.
Sunday 2/25 8pm — We arrived at the hospital for the third Sunday in a row. We were less excited, and now emotionally fatigued than the times before but we were here to do it.
I am 1cm dilated and 60% effaced for the last four weeks.
Delivery begins at 100% effacement and 10cm dilation.
Sunday 2/25 11pm — Induction started with a vaginal misoprostol which is meant to release prostaglandins to support early labor cervical dilation (1-4cm). They only give the minimal dosage to not overload the uterus with contractions. Many times, women get this medication and they tip into natural labor. That was my hope.
The doctors kept asking if I felt the contractions as they were monitoring that they were pretty strong and close together. To me, it was nothing more than I had already experienced at home for the last month. I thought this was easy.
Monday 2/26 1am — I was only progressed to 2cm. The doctors wanted to move on with the next layer of induction: a Foley Bulb Induction. This is a tube-like balloon that helps efface and dilate the cervix.
But I fought this suggestion to see if I could progress naturally later that morning. I wanted to wake up, fuel with food, and walk around with the contractions, letting the baby’s head with gravity push down to open me. Little did I know this wasn’t nearly possible.
Monday 2/26 11am — my partner was encouraging the next layer of induction while I was still hanging on to every chance I have for the most natural progression of labor. I was frustrated. Would a doula or mid-wife had been able to guide me better? Who knows.
I had previously mentioned to my partner the likelihood of ending in a cesarean section when interventions begin. We were doubly made aware of this during one of our previous trips to triage by a more natural-minded nurse. I had read a lot about this in Ina May Gaskin’s work “Natural Guide to Child Birth”.
These endings are more likely because induction is truly forcing the body to move into labor when maybe it’s not ready to. When the body is forced, it can create friction, tension, and stall labor progression. In order for the body to open—in any context, the body needs to feel safe, at peace and relaxed. Induction can take that peace away, pain can take that peace away, someone controlling your labor, can take that peace away.
A Turning Point.
Monday 2/26 1pm — I felt like I was running out of time, the doctors wanted to move me along with the bulb. The contractions were going, I was moving around, but there was no progression.
I eventually caved for the Foley Balloon and the resident doctor on shift first had to perform a cervical check—which he utterly failed in the process. The nurse on shift had to double check his work….pretty much do it for him. This felt violating and hurtful from both persons. I’ve had cervical checks that have not hurt before if the OB knows what they’re doing. Little did I know the lack of experience this resident had.
He’s now prepping for the balloon placement, a procedure that should have taken less than two minutes…took over five.
At this point I was squirming on the bed, unrelaxed, two different peoples hands inside of me grabbing at my most precious bits, tears starting, alone as I had encouraged my partner to check on our house and get a proper shower. I’m just feeling like something wasn’t right. The nurse asked me if that was traumatic for me…trembling, I gave no answer and asked for some space.
Monday 2/26 2pm — The resident doctor asked if I would like him to try again or if I would like someone else to attempt placement.
I asked the resident, “How many balloons have you successfully placed?” He responds with, “Three successful placements.”
OH REALLY?!
I politely opted for another resident, the one who was in emergency c-section. If the other doctor was in an emergency surgery, he surely could place a plastic foley into my cervix.
3pm — The second resident came in to place the balloon, explained that the balloon naturally encourages the body to produces more prostaglandins. This fact is something the other doctor failed to mention which would have helped in my decision process earlier on while fighting the cascade.
So the second resident finished the procedure within 90 seconds. By this time, I am fatigued, feeling tired, and my contractions were more painful. I labor through the pain with wailing, moaning, breathing, relaxing. I wasn’t even in the stages of “active labor” where pain is most common. Reminding myself with every contraction was safe to open up. Nothing budged for hours.
5pm — I made my way into the jetted tub which I was so excited my hospital had, but at this point I felt morally defeated, tense, tired, decision-fatigued, and alone despite my partner’s support.
6pm — My OB walked through the door at the start of her night shift and sat on the side of the tub, grabbing my hand, compassionate as ever. I was naked, fully vulnerable, and I began to cry— it was an incredible relief to see her, to feel held by her. She supported me as I confess to her how disappointed I felt that day and that I truly don’t think I can do this any longer, that I was going to need more help.
We were coming up to 24 hours with 1cm of progress, something else needed to be done.
My doctor mentioned the resident that day was a substitute for someone she trusted. So she rallied a team together and assigned specific nurses and doctors to me for the evening. I felt seen and supported. The following team members changed everything for me and felt like family for the remainder of my stay.
The order for the epidural was placed.
8pm — Monday evening, my freedom and natural birth opportunity was over by choosing the epidural.
I remember reading about epidural stories and how women actually progressed in their labor with this option because they were relaxed and less tense.
With the epidural, you’re bound to the bed and can’t walk and so a foley catheter is placed in the bladder, this contraption lets your bladder release as needed. Little did we know this was also going to be a problem.
Tuesday 2/27 2am—Finally getting some sleep, I felt the balloon “pop” and with a cervical check, I am 3cm and 100% effaced. Progress was made!
Tuesday 2/27 5am—Pitocin started through an IV. Pitocin is fortified oxytocin, the love and bonding hormone, signaling the endocrine system from the pituitary gland to the uterus and cervix to open and dilate.
This process progressed me to 5cm cervical dilation and my water broke.
Meanwhile, my blood pressure began to drop. Baby was doing well throughout the process.
But they started giving more meds to fight the low blood pressure and pumped fluids to increase my blood volume…1,000mL, 2,000mL.
However, the nurse is concerned as she realized I am not releasing this fluid through my bladder. The fluid started dispersing to all other areas of my body.
Something was not right.
Additionally, I was feeling an increase in pain on my left hip. Knowing baby was positioned on my left side, there was so much pressure there. Even with the epidural I went from 0/10 pain to 12/10 pain in minutes. Pain I hadn’t felt since I tore my ACL in 2017.
I was screaming for more fentanyl, I could not handle whatever pain was happening. Cue the first booster to the epidural typically known as a bolus.
Tuesday 2/27 7am — My partner was scheduled for his final medical treatment at the facility next to the hospital we were at. This was the last of eight treatments that he’s gone through since December 2023. It makes him SO tired, after treatment, he returned and he slept for hours. We were really being tested here.
Tuesday 2/27 11am — I am finally 9cm dilated. Overloaded with more fluid, about 3,000mL pumped into me and little to none coming out through the bladder catheter. Pain really started to kick in on my left hip…yet again.
Screaming and wailing in pain, I beg for another bolus of fentanyl. Baby’s heart rate was tracking fine through this whole process, distress for him seemed minimal.
After the bolus, I begin vomiting from the drugs, and my partner woke up from his deep sleep as if he forgot where he was.


Tuesday 2/27 2pm — I opted for a third bolus of the fentanyl as the pain is so incredibly difficult. Pain that wasn’t a typical laboring pain. This was pain that is considered “back labor” which is when the baby is positioned in such a way that it causes immense pressure on one or both hips. I remember screaming one minute and drifting off into opiate land in another. But once I got oriented after the third round of medication, it was time to push.
I was 10cm, bod ready. Partner was alert. It’s go time.
Tuesday 2/27 4pm —I’ve now pushed for 2.5 hours.
My entire pregnancy, I let my partner know I didn’t want to push on my back. He advocated for me but ironically, it was the position I felt the most progress for baby’s descent.
However, baby wasn’t really descending push after push.
I had two very trusted doctors working with me that day. My OB’s doctor and the man who placed the ballon. Each doctor had their hands inside of me at the lips of my cervix, trying to turn the baby in the pelvis as they realized the positioning was strange and causing a stall in descent.
The doctors both mention, “With the way you’re pushing and your breathing, this baby should have come out within 20 minutes…something is not right and we can’t get him to come out…” They knew he was head down. Prior to induction he presented sunny side up for the first time ever, doctors told me baby’s usually turn during labor and positioning is not something to worry about. But clearly, something about labor progression was not right and my intuition around his positioning was right (re: Part 1 at the appointment with my OB’s colleague).
I had a feeling the baby’s position was keeping my labor from progressing since the early day’s of prodromal labor in late Janurary. I had a feeling that this was the cause for many, many contractions and no cervical dilation over time. What if the cord was wrapped around his body? What is anatomically wrong that we could not see?
They both advised, “This is when we typically recommend a cesarean section.” The words no natural minded person wants to hear. I could have fought for continuing to push but again, I was adding up what I knew about my baby, my body, and this process. I knew all along something was not aligned. If I chose to maybe force the descent, I would lose the medical team I worked with all day to the next team on the following shift or I would potentially hurt the baby.
Tuesday 2/27 5pm— I called my partner who left the room as the nurse reminded him to go eat some food as he hadn’t eaten all day. I let him know we we’re opting for surgery. His heart dropped, everything I had been fighting for and educating him on throughout pregnancy was coming true. I’ve been through two surgeries before, I knew I could handle this and I knew I wanted to bring the baby into this world without forcing what I couldn’t see.
Ultimately, after 41 hours, baby Hayden entered this world by c-section rolling in at 8 pounds and 12 ounces.
When my partner showed me pictures of my baby, the first thing I said was “He looks like my dad!!” (more to come on this).
I was quite demanding to the medical team to see my child because the hospital prides itself on the Golden Hour which is non-interventional alone time with your baby for one hour after birth, yet they were intervening because this wasn’t a simple or vaginal birth. When I finally got to hold him, I soothed his third eye immediately.
As I used to connect us while he was in the womb with the words: “I’m right here, I’m right here.”
In post operative recovery, we were flooded by more medical professionals that I had never met before, in all mothering instinct, I demanded they leave me alone and let me be with my baby.
I was losing consciousness—my blood pressure was tanking to 71/38—I was in deep danger medically from all the fluid my body was holding on to.
Hayden’s head had been compressed on my bladder, not allowing the fluid to enter and release, it was all stored in my veins and tissue. Primitively, all I could focus on was getting my baby to latch and breast feed, letting our connection bond deeper.
Thursday 2/29 11am— We were being discharged from the hospital and while I felt utterly cared for by most of my medical team, I still felt uncertain as to why I ended in cesarean.
About 15 of 25 people that discharged us made a comment on how large my baby’s head was. He was measuring in the 88th percentile.
I came across a midwife who approaches child birth more naturally than obstetricians and asked her a few questions in hopes to put my anxiety to rest.
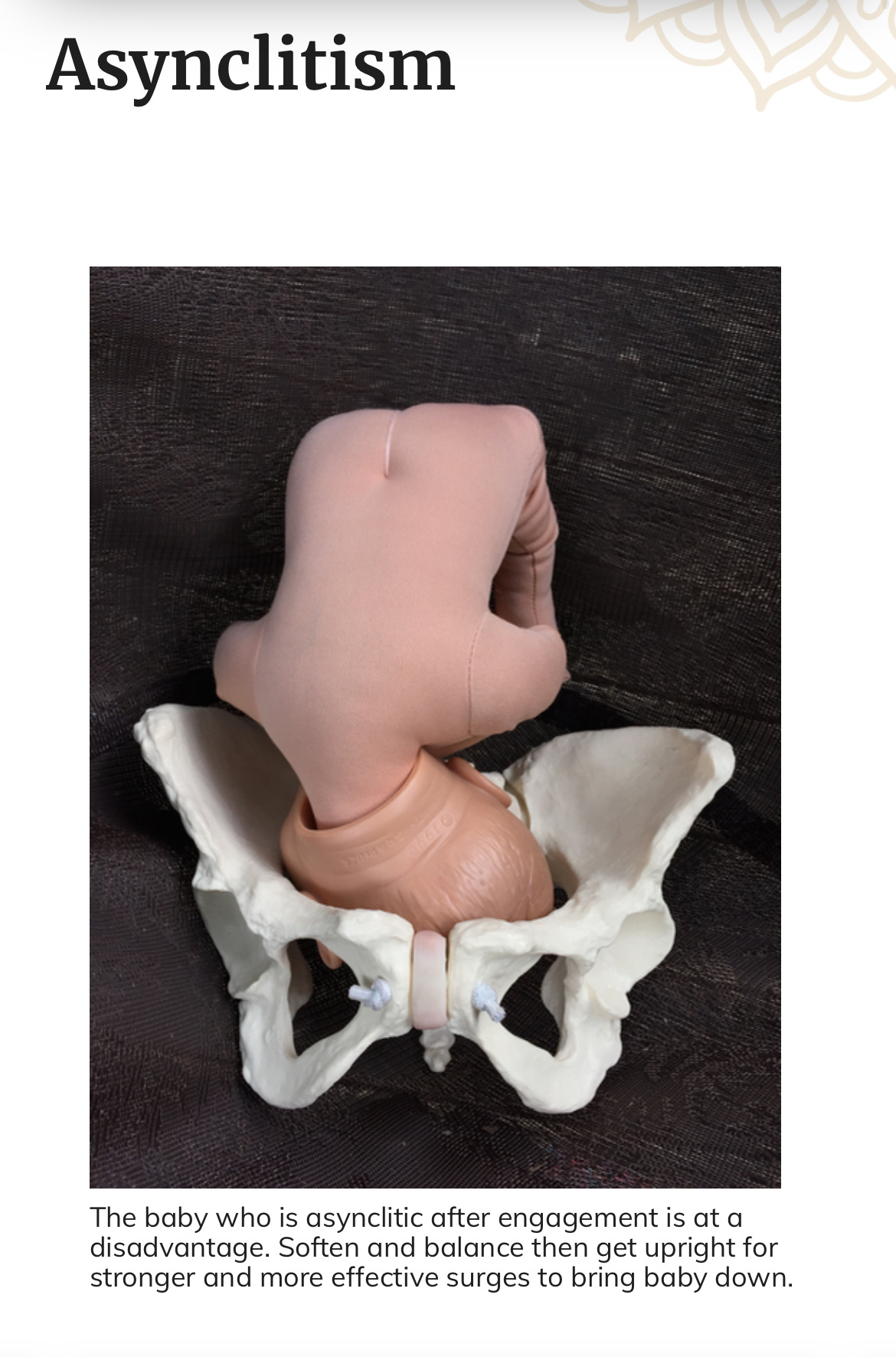
She mentions that it sounded like the baby was in Asynclitic position. This is a tilted head and body in the womb that makes it virtually impossible to brith vaginally. Lots of repositioning prior to labor is required which no one truly encouraged before or during labor. See the image of the baby’s angle below. This is where knowing what I know now, I would have opted for additional support for optimal positioning.
Acceptance and What I Know Now
Ultimately, it was hard to accept a surgical birth, it was hard to accept that I had to be induced, but I chose that. The small whisper inside of me knew the baby was in a challenging position even before I went to my final appointment. I had this feeling because I was experiencing a lot of start and stop labor but seeing little progression. I had this feeling because myself and all my loved ones were convinced the baby was coming in early February. I had this feeling that urged me to ask my doctor about induction. I had this feeling because he was changing into a less desired position at the very end of pregnancy.
I am glad I listened to my intuition to be at the hospital as opposed to a home birth. I am glad I made the decision to enter induction and I am glad I did it with the opportunity to have my doctors support. I am glad I had the epidural to shield the pain for the prolong labor.
For the situation I was in, I was glad. Could it have changed if I was in another situation, if I had different support? Maybe. But lingering in shoulda, coulda, woulda, doesn’t help. I’ve had to accept that this was my situation, this is the path we took.
Every path taken is okay, we can always try differently next time.
Life is a learning process.
Knowing what I know now
Positioning can and should be important before labor begins.
It would be important to have someone on your medical and advisory team who advocates for optimal positioning to allow labor to be as natural and enjoyable as possible.
I do wish I had invested in a midwife and a physical therapist throughout pregnancy to be with me and educate me in all aspects of what it means to give birth: medically, physically, mentally, emotionally, and energetically.
I know I have uneven hips from post surgical recovery after my ACL reconstructive surgery. I’ve heard it many times before. This is my trauma passed onto my baby—not a bad thing, but something I can support him in as we heal this now, together.
Ultimately, as an alternative practitioner myself, I vow to commit to working with a team of various individuals that are experts in their craft. Not just a doctor. Not just relying on my own knowledge. If we’re learning anything in this day and age, one way is not the only way. The way is multi-faceted and should be invested in as so.
The lessons I learned from this process are:
Invest in professionals in all four aspects of being human. Not to have control, but to continue to develop in all the ways for the best outcomes possible.
Invest in education for both you and your partner, practice conversations and actions together.
Trust yourself and your intuition no matter what. Let the process unfold.
However you birth your baby is the right way for what it is and comparison of processes or hatred for eastern or western perspectives is a waste of energy—they all have a place.
I tried the natural route, I tried the epidural and vaginal route, and I tried the surgical route.
What matters is: I am with my baby.
What matters is: life is a relationship to a work in progress.
No matter what happens: intuition is the utmost important tool you can develop.
The rest will come.
The Spirituality
After I came home and journaled about the process of my birth, I opened my note book to find the last oracle card that I pulled before labor. I was desperate for answers. I gave up on trying to adjust my perspective or understand what was happening and this was the final card I pulled on 2/13.
As I open the journal at home in recovery, this card pops out:


The Sacred Scar.
Your inner and outer scars are marks of your soul’s courage. They are signs of strength and survival, of your willingness to be alive. Which once caused pain can be transformed into higher knowledge and inner power. Trauma shall be transformed through spiritual initiation, leading you from woundedness to wisdom. You have nothing to be ashamed of.
Alanna Fairchild
I have yet to find a settled clarity as to why I am here to tell this story. Other than the fact that no matter how you birth is okay.
Ultimately, I settle into: no amount of trauma can be too much for the right amount of unconditional love.
After healing and processing my birth story for myself, I am able to heal and support my child. I witness breaking the chain before my very eyes.
It takes deep inner work, being with the Self, and using the light of the spiritual components to truly transform trauma into wisdom.
This is my life’s work.
Though the body is a temple, it’s only temporary.
Welcome to the World Hayden James 🕊
We’re right here. You’re mine now.
Xx







Thank you for sharing your birth story with your community. I admire your courage, strength, intuition and so much more. I am someone who hasn’t entered motherhood yet and I feel so grateful to have your story as a resource. Thank you Erin for paving the path of vulnerability. I cherish you and I am so proud of you!!
With love,
Em